2024 Concussion Guidelines PLUS how and when to return to sport after concussion
Buckle in, this blog is a long one! We tried to condense it but feel that all of this info is important and want this to be a thorough resource that you can come back to.
2024 AFL Community Concussion Guidelines
While many athletes appear to recover quickly from a concussion, there is growing body of evidence and awareness of the long-term impacts of concussion. It can be a really stressful time for parents, athletes and coaches to decide how and when a player returns to sport. Currently the motto is “if in doubt, sit it out”, however a clearer message may be more helpful when explaining timeframes to athletes.
Our message is: have a thorough assessment with a concussion trained health professional and agree on a return to play plan so that all parties can make an informed decision about when an athlete is ready to return to sport.
Understanding the latest guidelines will also make it easier to resist any pressure to return too quickly - whether that be from the athlete themselves, a coach or well-meaning family members.
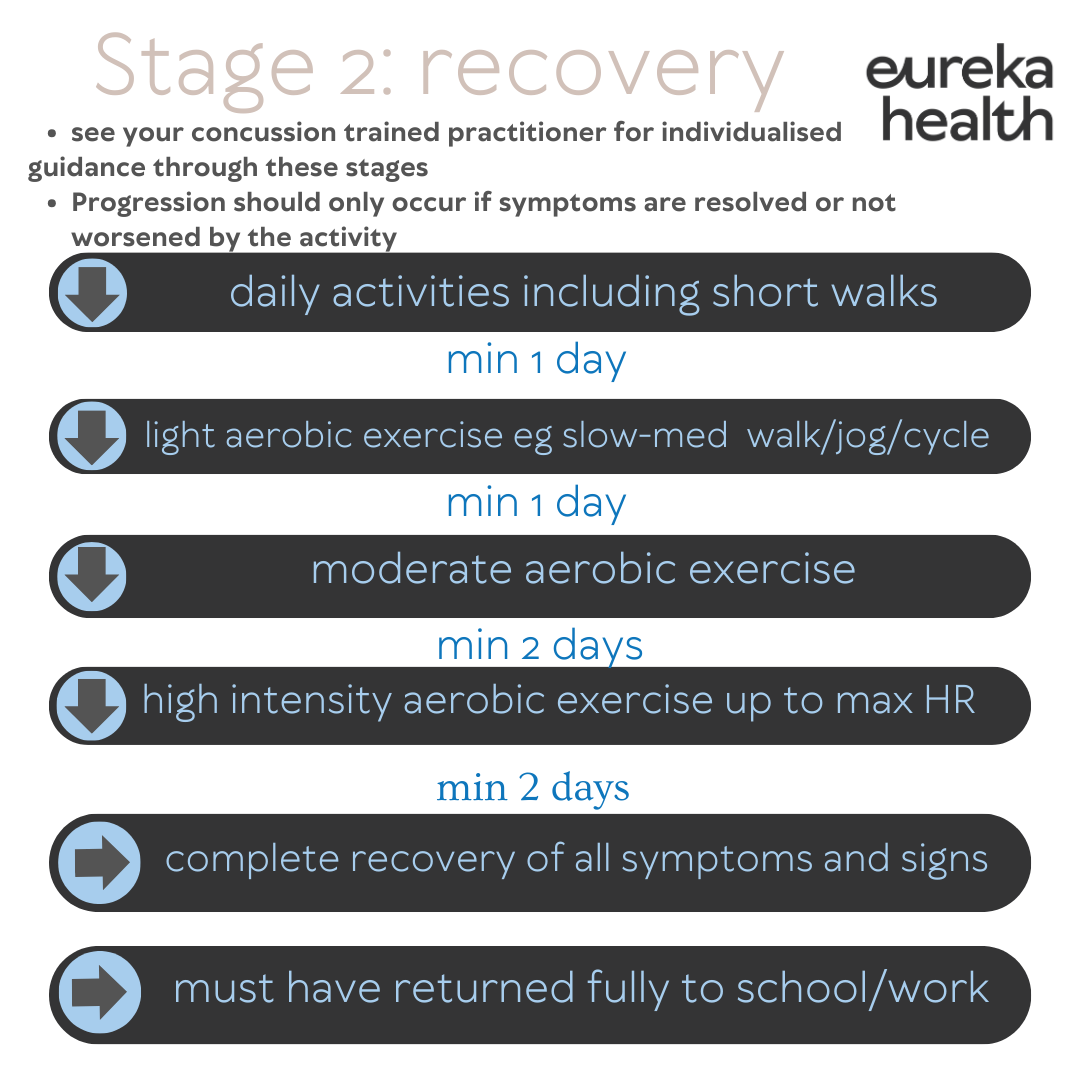
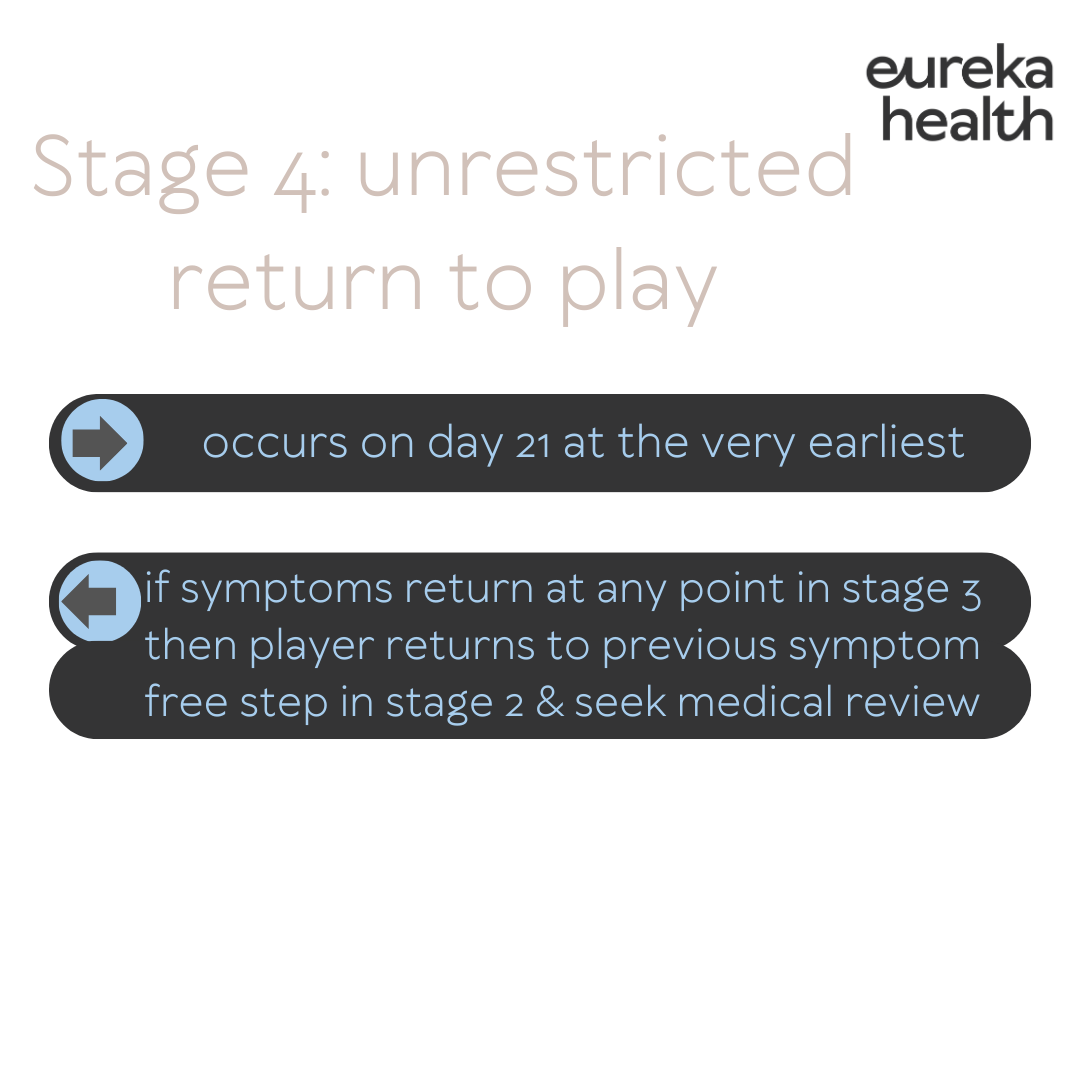
Under the new community AFL guidelines, the earliest that a player can return to play after a concussion is on the 21st day after the day on which the concussion was sustained - provided that the player has safely progressed through each phase of the return-to-play program (details below).
For example, if a player suffers the concussion playing in a match on a Saturday , this is counted as Day 0. Day 1 is the day after the match (Sunday)
The player will, at a minimum, miss the next 2 Saturday games and at the absolute best case scenario, might return to play on day 21 (the third Saturday in this example). This best case scenario assumes that the athlete has safely progressed through the 3 stages of the protocol and been approved by their medical practitioner to return to play. If it’s hard to picture a graded rehab program for your brain, we encourage you to picture the classic hamstring strain. Sometimes a low grade hamstring strain might be a 21 day injury, be we definitely don’t spend three weeks completely resting! Those three weeks always include gradual strengthening, loading the hamstring in different ways and gradually adding in different elements of training before the final clearance that you’re ready to play.
The return-to-play program consists of three distinct stages – rest, recovery and graded return to training and play. The updated guidelines insist on a minimum period of 24 hours (or longer) for each step of the progression and, if any symptoms recur during the graded return to training and play stage, the player athlete must go back to the previous symptom-free step. Our clinicians can tailor a rehabilitation program to guide you through these steps at an appropriate pace.
The guidelines also insist on an individualised approach to return to play where factors such as young age (i.e., 18 years or younger), where there is a history of learning disorders or mood disturbance that may impact on monitoring of recovery, or a history of multiple concussions, may necessitate a more cautious and conservative approach. A history of migraines or chronic neck pain may need extra attention too - most concussions will come with a neck injury that requires assessment and treatment.
The player must have medical assessment prior to being cleared to return to full contact training with the group and then a further medical assessment before being cleared to return to play.
WHAT IS CONCUSSION?
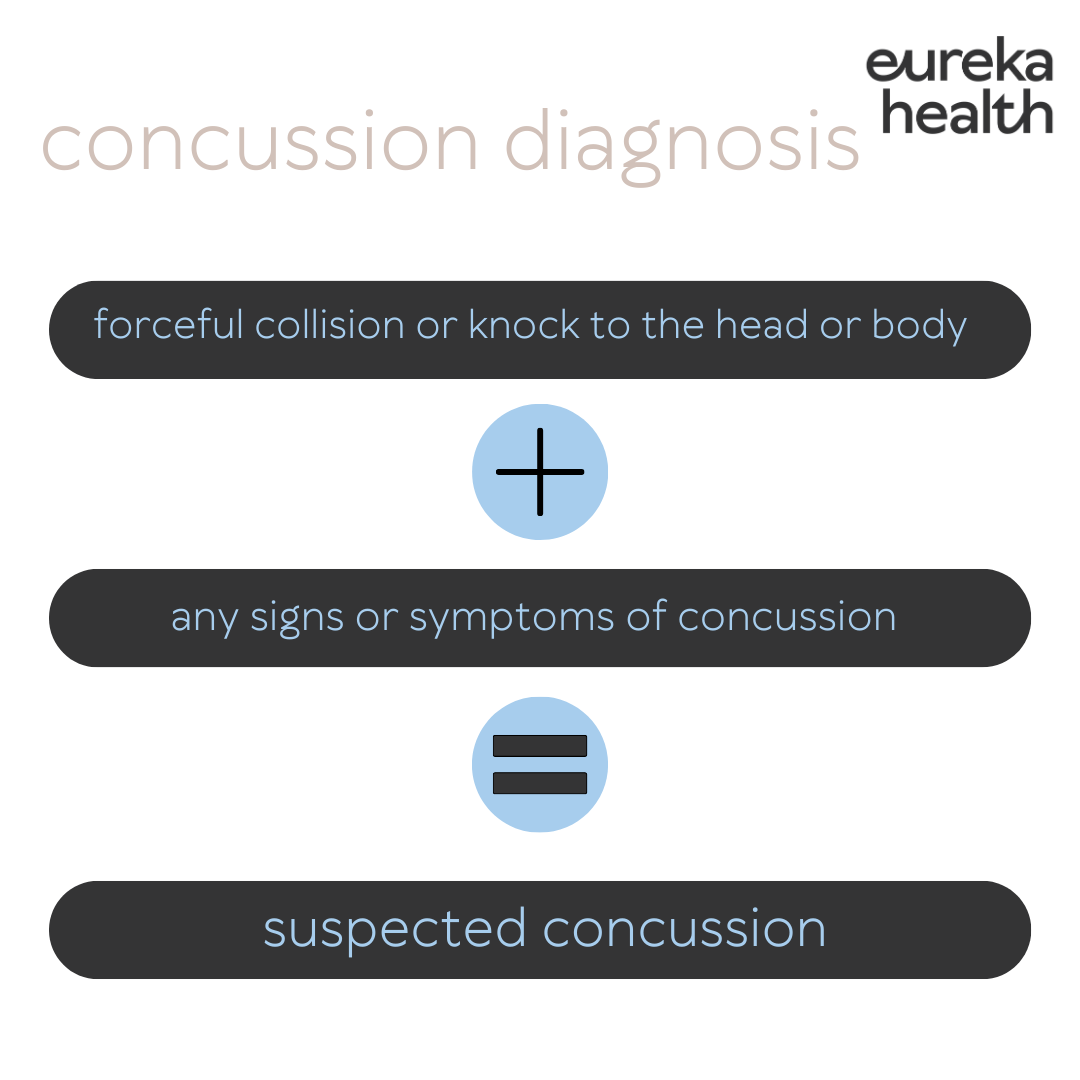
A concussion is an injury to the brain that results in temporary loss of normal brain function. It causes short lived neurological impairments and symptoms may evolve in the hours or days following the injury.
Concussions can be caused by direct trauma to the head – e.g. collisions with other athletes or being hit by a ball or ground. They can also occur as a result of rapid acceleration-deceleration of the head, such as in whiplash injuries or other seemingly innocuous incidents.
Many people assume that concussions involve passing out or a loss of consciousness, however the majority cases of concussion never involve a loss of consciousness.
If managed appropriately, most symptoms and signs of concussion resolve spontaneously. However, complications can occur, including prolonged symptoms and increased susceptibility to further injury.
A great way to think about concussion and it’s affects on the brain is that it causes an “Energy Crisis”. The trauma to the brain results in a decrease in cerebral blood flow due to blood vessel spasm, reducing the supply of glucose/energy available. When concussed, brain function (particularly vision and vestibular/balance/co-ordination), is inefficient and the lack of energy available for the brain to use can lead to fatigue, irritability, frustration and anxiety. This energy crisis is the main reason for concussion symptoms and is why early guided management is so important. This “Energy Crisis” is thought to take up to 14 days in adults to resolve and up to 30 days in children and teenagers.
SYMPTOMS OF CONCUSSION
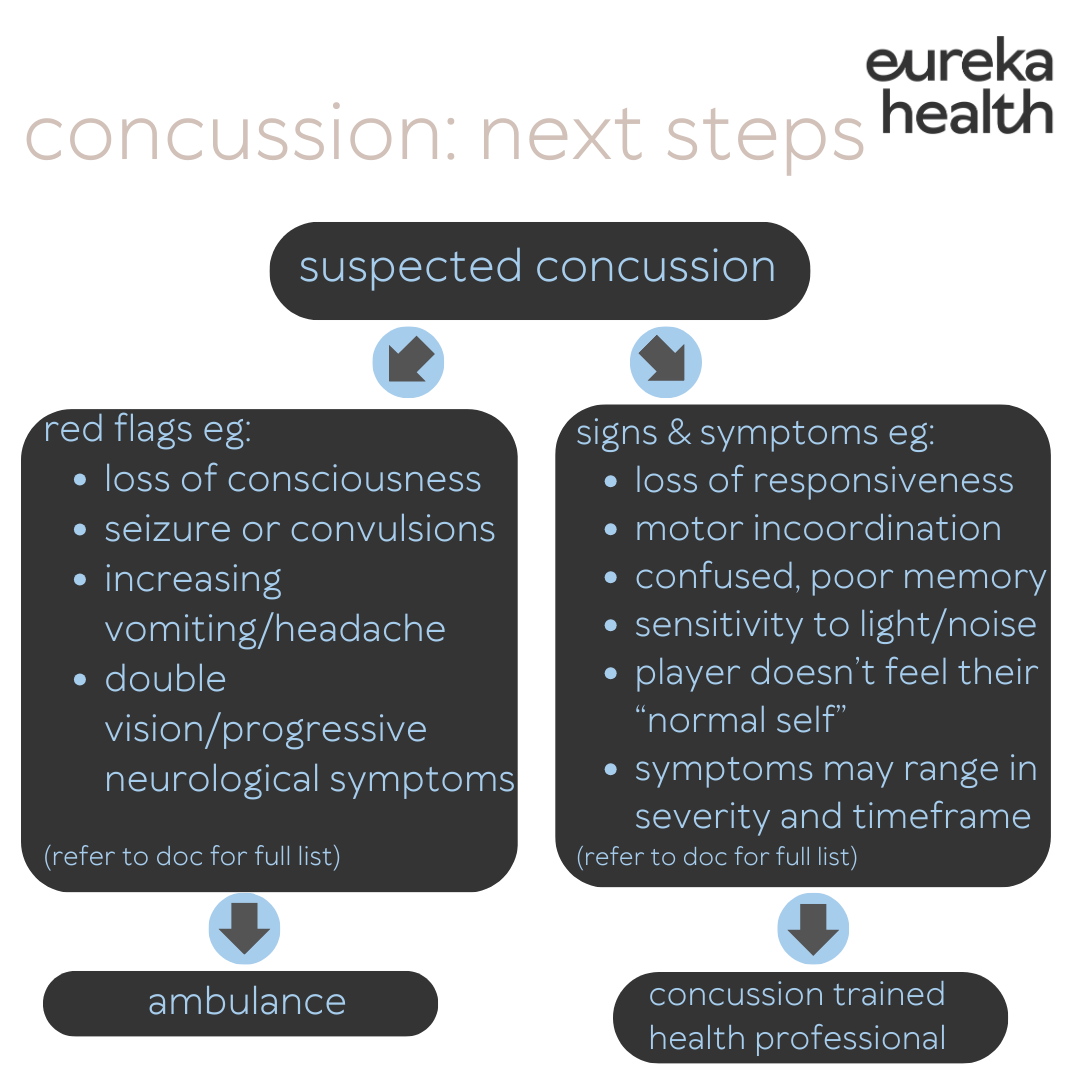
While some symptoms are obvious, others can be difficult to recognise. The athlete is often not the best person to be assessing for symptoms – parents and partners need to be on the lookout for subtle and non-specific symptoms. Sometimes symptoms can be obvious immediately and others can take a while to emerge.
The Sports Concussion Assessment Tool (SCAT6) lists 22 possible symptoms that include confusion, blurred vision, drowsiness, balance problems, light sensitivity, irritability, headache, neck pain and sadness among many others.
ONGOING ISSUES ASSOCIATED WITH CONCUSSION
Following a concussion, some people may suffer persisting symptoms for weeks to months. This is known as post-concussion syndrome. Patients with post-concussion syndrome should avoid activities that put them at risk for a repeated concussion. The advice is very clear: athletes should not return to play while experiencing these symptoms. It is critical that these patients are assessed by health care practitioners trained in concussion management and rehab.
Second impact syndrome is the biggest risk associated with concussion results from acute and often fatal brain swelling that occurs when a second concussion is sustained before complete recovery from a previous concussion. The impact is thought to cause vascular congestion and increased intracranial pressure, which can occur very rapidly and can lead to coma and death. Current evidence shows that children and teenagers are more at risk of this; hence the time out from contact training and sport is consisdered. to be so important in the management of concussion.
ATHLETE CARE & RETURN TO PLAY GUIDELINES
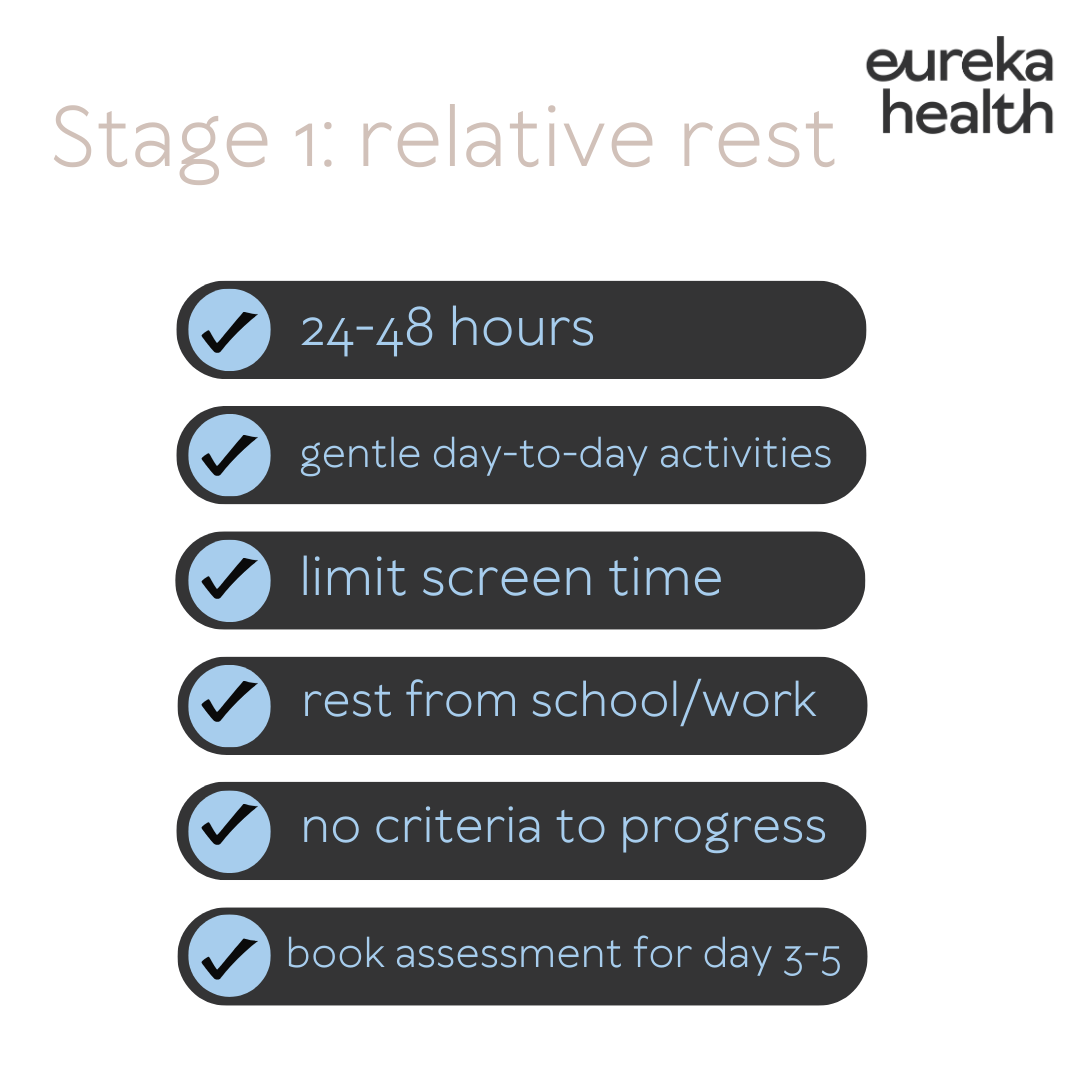
As well as the symptoms associated with the actual concussion, there may be conflicted feelings of wanting to return to their chosen sport but also a fear of long-term consequences. All athletes need a thorough examination and treatment plan as well as rest and careful monitoring. We cannot emphasise enough how important rest is in the recovery phase. By rest, we do not mean go into a dark room and lay in bed until symptoms are gone - this is more likely to lead to post-concussion syndrome/ongoing symptoms. Rest is recommended for the first 24-48 hours but then light aerobic exercise is encouraged: a few walks outside if tolerated or some gentle spinning on a stationary bike. Return to work or learning, as well as pacing of increasing exercise is guided by each individual’s symptoms. The guidance from health care practitioners trained in concussion management and rehab can be extremely helpful here and can help lead to a full recovery.
The AIS return to sport protocol for community and youth sport includes:
Introduction of light exercise after an initial 24-48 hours of relative rest.
Several checkpoints to be cleared prior to progression (this differs slightly from the AFL guidelines).
Gradual reintroduction of learning and work activities. As with physical activity, cognitive stimulation such as using screens, reading, undertaking learning activities should be gradually introduced after 48 hours.
At least 14 days symptom free (at rest) before return to contact/collision training. The temporary exacerbation of mild symptoms with exercise is acceptable, as long as the symptoms quickly resolve at the completion of exercise, and as long as the exercise-related symptoms have completely resolved before resumption of contact training.
A minimum period of 21 days until the resumption of competitive contact/collision sport.
Return to learn and work activities should take priority over return to sport. That is, while graduated return to learn/work activities and sport activities can occur simultaneously, the athlete should not return to full contact sport activities until they have successfully completed a fully return to learn/work activities. We can help to guide you or your child through this process.
Strong evidence exists regarding the benefits of physical activity and aerobic exercise treatment as early interventions.
Limited evidence exists on SRC (Sport Related Concussion) in patients aged 5–12 years.
To book a concussion assessment and return to play program with one of our clinicians, click here
References:
2024 AIS Concussion & Brain Health Position Statement: https://www.concussioninsport.gov.au/__data/assets/pdf_file/0004/1133545/37382_Concussion-and-Brain-Health-Position-Statement-2024-FA.pdf
2023 International Consensus update: https://bjsm.bmj.com/content/57/11/695
Concussion in Sport Aus Gov: https://www.concussioninsport.gov.au/
NFL Concussion Guidelines: https://www.nfl.com/playerhealthandsafety/health-and-wellness/player-care/concussion-protocol-return-to-participation-protocol
Sports Medicine Australia: https://sma.org.au/resources-advice/concussion/
2024 AFL Community Guidelines: https://play.afl/learning-resource/afl-community-concussion-guidelines#article-1
Resources:
CRT6: https://bjsm.bmj.com/content/bjsports/57/11/692.full.pdf
SCAT5 kids: https://bjsm.bmj.com/content/bjsports/early/2017/04/26/bjsports-2017-097492childscat5.full.pdf (Note SCAT 6 has been
Child Scat 6: https://bjsm.bmj.com/content/57/11/636
SCAT 6 Adults/over 12s: https://completeconcussions.com/wp-content/uploads/2023/06/SCAT6.pdf